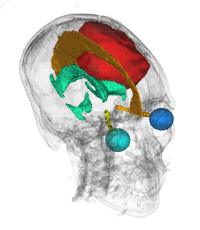
 In radiation therapy, the delivery of a radiation dose to the treatment target is very conformal, with as low as 1 mm uncertainty. Therefore, the definition of the target itself becomes critical. The target for irradiation is defined as the gross disease visible on medical images plus a margin that accounts for the microscopic "invisible" spread into surrounding tissues. The margin defines the boundary of the clinical target volume (CTV). In very conformal treatments, a higher risk of treatment failures could be attributed to inaccurately defined CTV. The CTV boundary is determined by anatomical structures that are natural barriers to the spreading of tumors. For gliomas, which are the most common brain tumors, the boundary is defined by the falx cerebri, tentorium cerebelli, brain sinuses, and ventricles. The correct placement of the CTV boundary can spare a measurable amount of brain tissue from radiation, which will in turn reduce the risk of post-treatment neurocognitive deficit.
In radiation therapy, the delivery of a radiation dose to the treatment target is very conformal, with as low as 1 mm uncertainty. Therefore, the definition of the target itself becomes critical. The target for irradiation is defined as the gross disease visible on medical images plus a margin that accounts for the microscopic "invisible" spread into surrounding tissues. The margin defines the boundary of the clinical target volume (CTV). In very conformal treatments, a higher risk of treatment failures could be attributed to inaccurately defined CTV. The CTV boundary is determined by anatomical structures that are natural barriers to the spreading of tumors. For gliomas, which are the most common brain tumors, the boundary is defined by the falx cerebri, tentorium cerebelli, brain sinuses, and ventricles. The correct placement of the CTV boundary can spare a measurable amount of brain tissue from radiation, which will in turn reduce the risk of post-treatment neurocognitive deficit.
The quality of the treatment plan is determined not only by the precise placement of the CTV boundary but also by the accurate delineation of healthy structures that must be spared from receiving the radiation dose. These structures are routinely outlined for each treatment plan; therefore, automation will improve both efficiency of the plan creation workflow and consistency of the structure definition.